Synovial Fibroblasts (SFs) are cells that make up part of the connective tissue, or synovium, around human joints. In RA patients, SF cells cause damage by invading and attacking the cartilage and bone around the joint
A study reveals the key role of different types of fibroblast cells in the development of rheumatoid arthritis (RA), opening up a new avenue for research into treatment of the disease. Synovial Fibroblasts (SFs) are cells that make up part of the connective tissue, or synovium, around human joints. In RA patients, SF cells cause damage by invading and attacking the cartilage and bone around the joint.
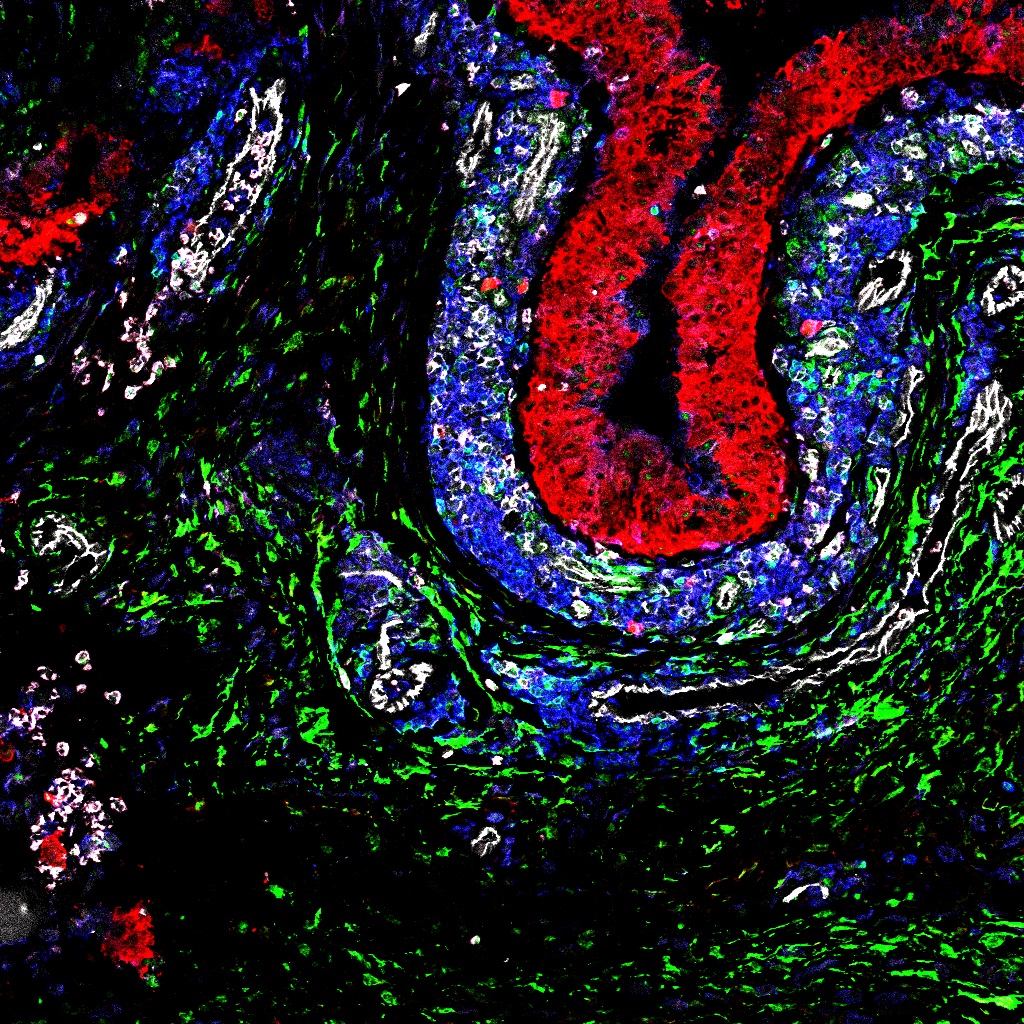
A team from University of Birmingham’s Institute of Inflammation and Ageing identified 2 distinct types of SF within the synovial membrane. The team showed that these cell types, defined by the presence of specific cell surface markers (PDPN and CD248), aggregate in different layers of the synovium, and just one (the PDPN type) is responsible for cartilage damage in RA patients.
SF cells from RA patients were grown in vitro within an artificial synovium, then ‘activated’ using cytokines. The artificial synovium with the SFs was then inserted into a mouse (whose own immune system had been ‘switched off’), along with human cartilage to simulate a joint, to see how SF cells would develop in vivo.
Following implantation, tests showed that the ‘lining’ layer of the artificial synovium (i.e. the part closest to the cartilage) contained invasive PDPN type SFs, while the part that was further away from the cartilage contained the non-invasive CD248 type. The study also confirmed recent findings that ‘activated’ SF cells can migrate, i.e. travel through blood vessels to attack other cartilage in the body. PDPN type SF cells were the first to migrate, with CD248 cells only appearing in secondary tissue at a later stage.
Dr Adam Croft said: “This study not only shows the existence of distinct sub-sets of synovial fibroblasts, but also suggests that these cells are able to self-organise into lining and sub-lining layers in the presence of cartilage. Combined with the difference in migration rates between the two types of cell, these results are extremely promising in terms of finding new therapeutic targets for treatment of rheumatoid arthritis.”
Current treatment for RA involves giving patients a combination of immunosuppressive drugs, which can have a serious impact on quality of life. The results of this study suggest that targeting SF cells processes could make future treatments not only more effective, but also more manageable for patients. http://www.birmingham.ac.uk/news/latest/2016/11/New-study-on-role-of-fibroblasts-in-rheumatoid-arthritis-gives-hope-of-more-targeted-treatments-for-patients.aspx






Recent Comments