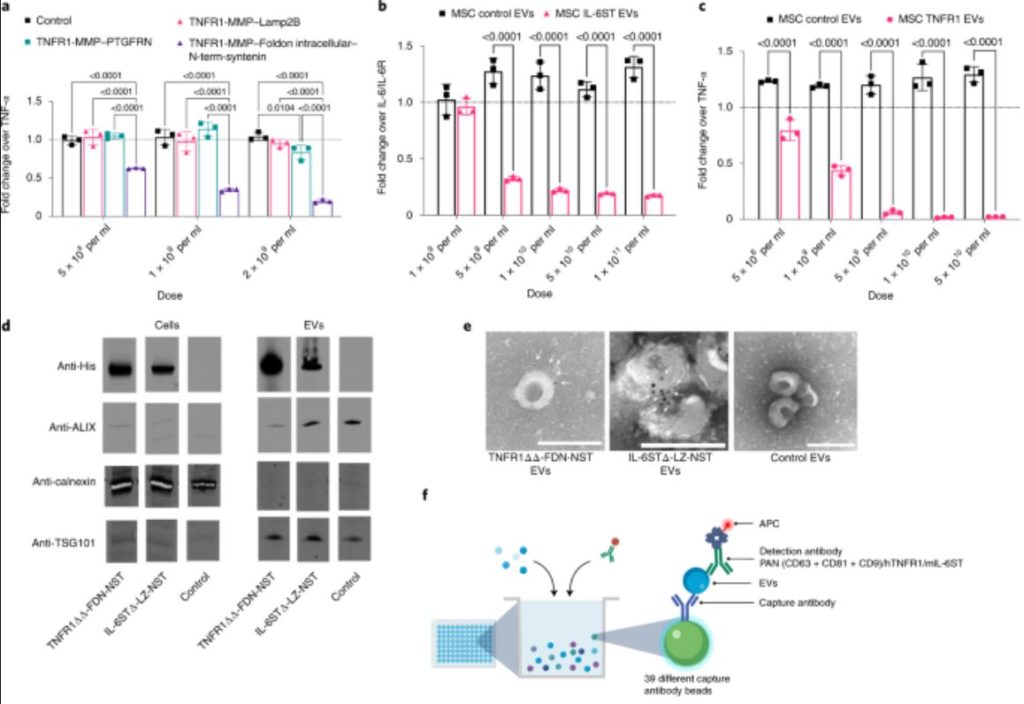
Scientists hope that tiny sacs of material excreted by cells — so-called extracellular vesicles — can be used to deliver drugs inside the body. Researchers at Karolinska Institutet now show that these nanobubbles can transport protein drugs that reduce inflammation caused by different diseases. The technique, which is presented in Nature Biomedical Engineering, shows promising results in animal models.
Extracellular vesicles (EVs) are important in inter-cellular communication as carriers of biological signals. They are nanometre-sized membrane-coated packages excreted by cells that can deliver fatty acids, proteins and genetic material to different tissues.
The tiny bubbles are f...
Read More






Recent Comments