
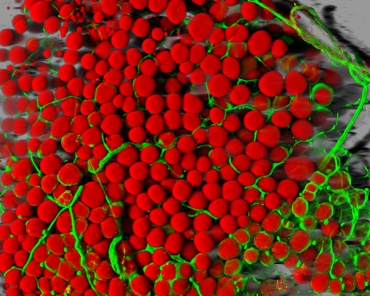
Postprandial macrophage-derived IL-1β stimulates insulin and both synergistically promote glucose disposal and inflammation. Nature Immunology, January 2017 DOI: 10.1038/ni.3659
When we eat, we do not just take in nutrients – we also consume a significant quantity of bacteria. The body is faced with the challenge of simultaneously distributing the ingested glucose and fighting these bacteria. This triggers an inflammatory response that activates the immune systems of healthy individuals and has a protective effect, as doctors from the University and the University Hospital Basel have proven for the first time. In overweight individuals, however, this inflammatory response fails so dramatically that it can lead to diabetes.
It is well known that type 2 diabetes (or adult-onset diabetes) le...
Read More





Recent Comments