Scientists discover role immune system’s T cells play in regulating fat and muscle loss during infection in mice. Scientists discovered that 1) the wasting response to T. brucei infection in mice occurs in two phases, each regulated by different immune cells and 2) fat loss did not benefit the fight against infection, but muscle loss did. The findings inform the development of more effective therapeutics that spare people from wasting and increase our understanding of how wasting influences survival and morbidity across infections, cancers, chronic illnesses, and more.
Although infections can present with many different symptoms, one common symptom is the loss of fat and muscle, a process called wasting. Salk scientists wanted to know whether wasting was beneficial in fighting infections.
“We oftenmake assumptions that conditions like wasting are bad, since they often coincide with higher mortality rates,” says senior author Ayres, Salk Institute Legacy Chair and head of the Molecular and Systems Physiology Laboratory. “But if instead we ask, what is the purpose of wasting? We can find surprising and insightful answers that can help us understand the human response to infection and how we can optimize that response.”
Defending the body from an invader requires a lot of energy. Prior studies suggested this immune-related energy consumption had the unfortunate consequence of wasting. But Ayres and team were curious to know whether wasting could be beneficial and not just a side effect.
Specialized immune cells called T cells are slow to respond to infections, but when they do respond, they adapt to fight the particular infection. Ayres was interested to know whether it was these T cells causing wasting. If T cells are responsible for the condition, that would indicate wasting is not simply an unproductive side effect of energy-hungry immune cells.
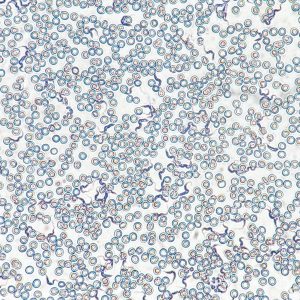
The cells of interest are called CD4+ and CD8+ T cells. CD4+ T cells lead the fight against infection and can promote the activity of CD8+ T cells, which can kill invaders and cancerous cells. The two T cell types often work together, so the researchers hypothesized their role in wasting may be a cooperative effort, too.
To work out the relationship between CD4+ and CD8+ T cells and wasting, the researchers turned to the parasite T. brucei. Because T. brucei lives in fat and can block the adaptive immune response — which includes T cells — it was a perfect model infection for their questions about fat wasting and how T cells mediate that process.
The team investigated 1) the role of CD4+ and CD8+ T cells during T. brucei infection and 2) how removing CD4+ and CD8+ T cells changed the longevity, mortality rates, parasite symptoms, and amount of parasite present in infected mice.
The researchers found that CD4+ T cells acted first and initiated the process of fat wasting. Afterward, but completely independently of the fat wasting, CD8+ T cells initiated the process of muscle wasting. The CD4+ T cell-induced fat wasting had no impact on the ability for the mice to fight T. brucei or to survive infection. The CD8+ T cell-induced muscle wasting, however, contrary to the traditional assumptions about wasting, helped the mice fight T. brucei and survive the infection.
“Our discoveries were so surprising that there were times I wondered if we did something wrong,” says first author Samuel Redford, a current visiting researcher and former graduate student in Ayres’ lab. “We had striking results that mice with fully functioning immune systems and mice without CD4+ T cells lived the same amount of time — meaning, those CD4+ T cells and the fat wasting they caused were completely disposable in fighting the parasite. And beyond that, we found that normally cooperative T cell subtypes were working totally independently of one another.”
The findings illustrate the important role of immune cells in both fat and muscle wasting and the necessity to understand the function of such responses to inform therapeutic interventions.
“We can learn so much about our immune systems by looking at the environments and infections we have co-evolved with,” says Ayres. “While T. brucei is an interesting and important case, what is exciting is extrapolating our findings to understand, treat, and overcome any disease that involves immune-mediated wasting — parasites, tumors, chronic illnesses, and so much more.”
In the future, the team will examine the T cell mechanism in other mammals and eventually humans. They also want to explore in more detail why muscle wasting is occurring and why CD4+ and CD8+ T cells play these distinct roles.
Other authors include Siva Karthik Varanasi, Karina Sanchez, and Natalia Thorup of Salk.
The work was supported by the National Institutes of Health (DPI AI144249, R01AI14929, NCI CCSG: P30 CA014195). https://www.salk.edu/news-release/why-we-lose-fat-and-muscle-during-infection/






Recent Comments