Researchers at Shanghai Jiao Tong University School of Medicine, China, have discovered that shutting down part of the innate immune system increases anti-tumor activity.
In a paper, “Noncanonical MAVS signaling restrains dendritic cell–driven antitumor immunity by inhibiting IL-12,” published in Science Immunology, the team details how exploring the role of mitochondrial antiviral signaling in tumor immunity uncovered unexpected insights into the relationship with immune responses and potential therapeutic implications.
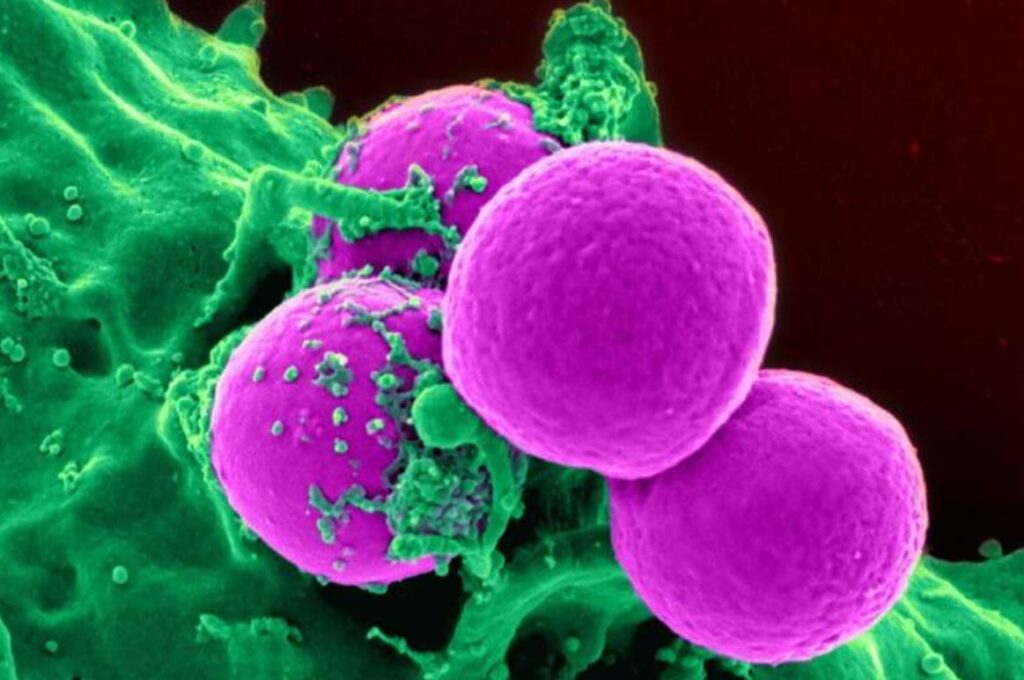
Mitochondrial antiviral-signaling (MAVS) proteins are part of the innate immune system encoded by the nuclear genome found mainly on the mitochondrial outer membrane. Considered a first line of defense against viral infections, they are rapidly produced upon viral recognition and quickly reduced when a virus is cleared from the system.
Contrary to its role in antiviral responses, the study finds that MAVS signaling may support tumor growth and impede anti-tumor therapy.
Deletion experiments found that MAVS deficiency in dendritic cells promotes explicitly anti-tumor CD8+ T cell responses without impacting other immune cell populations. These findings suggest that inhibiting MAVS signaling in dendritic cells could enhance anti-tumor immunity and improve current therapeutic approaches.
The loss of MAVS increased Interleukin12 expression by dendritic cells in the tumor microenvironment and draining lymph nodes. The loss also seems to affect the transit of tumor antigens to draining lymph nodes rather than affecting antigen presentation.
When combined with radiation, deleting MAVS led to synergistic tumor inhibition. This suggests that undeleted MAVS could contribute to radiation therapy resistance by impairing the maintenance of effector-like CD8+ T cells after radiation.
The findings propose that disrupting the MAVS pathway in dendritic cells could be a promising therapeutic strategy to enhance antitumor immune responses, particularly in combination with immunotherapies like radiation therapy.
The finding might also have interesting implications in non-cancer-related therapy. Severe cases of COVID-19 are associated with greater CD8+ T cell recruitment, and finding additional paths of CD8+ T cell activation in a COVID-19 scenario could be beneficial. https://medicalxpress.com/news/2023-12-innate-immune-cancer-therapy.html






Recent Comments